
We are currently witnessing one of the most exciting healthcare transformations. In the next 10 years, it may change as it has not done in the last several hundred years.
The reason for this change is the development of digital health markets. Accumulation of big data, artificial intelligence, smart wearables, telemedicine, etc. consistently accelerate digital health investments.
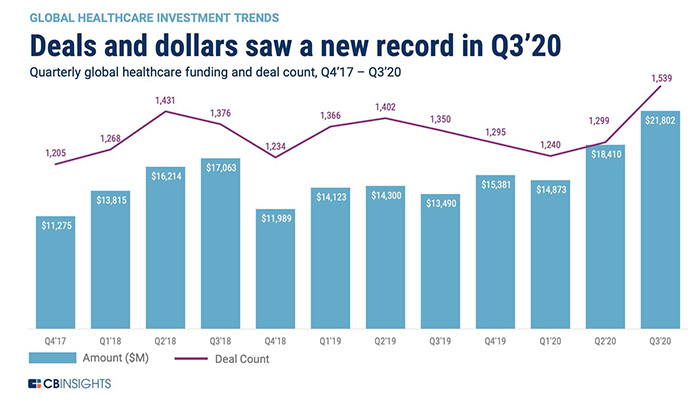
According to the latest CB Insights report, in Q3 2020 investment in this area reached $21.8 billion, which is 18% more than in the previous quarter and is an absolute maximum in this field.
Among health technologies, wearables and medical devices took the first place. They have attracted a total of $5 billion. The second place is for telemedicine: investments in this area have reached $2.8 billion. Artificial intelligence in healthcare is on the third place, such companies have raised $2.1 billion in funding. This is an all-time record for the entire history of CB Insights monitoring of this market since 2017.
The total volume of various sectors of the digital health market was estimated at $106 billion in 2019. According to Global Market Insights, it will grow by an average of 28.5% per year and in 2026 will amount to $639.4 billion.
Experts, startups and regulators are closely monitoring the development of digital health, relying on international analytical reports, scientific publications, etc. Many of this data contains rather specific terms and definitions that can be difficult for an unprepared reader to understand. We have prepared a short overview of abbreviations and terms used in digital health analytics to make it easier for our readers to navigate these difficult issues.
1. EHR, Electronic health record and EMR, Electronic medical record
Information systems for maintaining medical records of human health. EHRs are records of a patient's lifelong health, including outpatient observation. They may contain data from different sources, physicians and medical organizations.
EMRs are records of a specific hospitalization. In Russia, these terms are not distinguished, and the closest in meaning to a Russian term is EHR.
2. CDSS, Clinical decision support system
An information system that combines the clinical data of a particular patient with clinical guidelines and references in order to form personalized recommendations for a doctor on the correct tactics of patient management, including recommendations for diagnosis, treatment and patient monitoring.
3. ACO, Accountable Care Organization
According to Centers Medicare and Medicaid, ACO is an organization of health care providers that agrees to be accountable for the quality, cost, and overall care of Medicare beneficiaries who are enrolled in the traditional fee-for-service program who are assigned to it.
ACOs are part of the broader concept of population health management (PHM), which seeks to improve patient engagement and clinical proficiency while reducing costs. While ACOs don't entirely move away from a fee-for-service payment model, the focus shifts to creating savings incentives by offering providers bonuses for keeping healthcare costs down and meeting quality benchmarks. Conversely, healthcare providers who participate in an ACO and fail to meet the standards for cost control and patient care receive lower payments from Medicare.
4. MCO, Managed Care Organization
Managed care organizations are integrated entities in the healthcare system, which endeavor to reduce costs associated with healthcare expenditures. Since the 1970s, managed care organizations have shaped healthcare delivery in the United States through preventative medicine strategies, financial provisioning, and treatment guidelines.
A managed care organization (MCO) is a health care provider or a group or organization of medical service providers who offers managed care health plans. It is a health organization that contracts with insurers or self-insured employers and finances and delivers health care using a specific provider network and specific services and products.
5. PHM, Population Health Management
Population Health Management (PHM) seeks to improve the health outcomes of a group by monitoring and identifying individual patients within that group. Typically, PHM programs use a business intelligence (BI) tool to aggregate data and provide a comprehensive clinical picture of each patient. Using that data, providers can track, and hopefully improve, clinical outcomes while lowering costs.
A best-in-class PHM program brings clinical, financial and operational data together from across the enterprise and provides actionable analytics for providers to help improve efficiency and patient care. Delivering on the vision of PHM requires a robust care management and risk stratification infrastructure, a cohesive delivery system, and a well-managed partnership network.
6. VBC, Value-based care
Value-based programs reward health care providers with incentive payments for the quality of care they give to people with Medicare. These programs are part of our larger quality strategy to reform how health care is delivered and paid for. Value-based programs also support our three-part aim:
- Better care for individuals
- Better health for populations
- Lower cost
7. FFS, Fee-for-service
Health coverage in which doctors and other providers receive a fee for each service such as an office visit, test, procedure, or other health care service. The plan will either pay the medical provider directly or reimburse you for covered services after you have paid the bill and filed an insurance claim. When you need medical attention, you visit the doctor or hospital of your choice; the amount the plan plays may depend on whether the provider has a participation agreement with the plan.
8. HCIT, Healthcare Information Technology
Healthcare information technology (HCIT) is a term used to describe the use of computers in a clinical setting. HCIT's benefits include, but are not limited to: written electronic patient records, increased delivery of guideline-based care, easier access to investigation results, reduction of medical errors, and decreased rates of administration of potentially inappropriate care.
9. Precision Medicine
The tailoring of medical treatment to the individual characteristics of each patient… to classify individuals into subpopulations that differ in their susceptibility to a particular disease or their response to a specific treatment. Preventative or therapeutic interventions can then be concentrated on those who will benefit, sparing expense and side effects for those who will not.
10. Patient engagement
"Patient engagement" is a broader concept that combines patient activation with interventions designed to increase activation and promote positive patient behavior, such as obtaining preventive care or exercising regularly. Patient engagement is one strategy to achieve the "triple aim" of improved health outcomes, better patient care, and lower costs.
11. Healthcare provider
General term for any institution or member of the health care team providing health care. A healthcare provider is typically a hospital or clinic that provides an in or outpatient medical service or procedure.
12. Healthcare payer
A payer, or sometimes payor, is a company that pays for an administered medical service. An insurance company is the most common type of payer. A payer is responsible for processing patient eligibility, enrollment, claims, and payment. The Centers for Medicare and Medicaid Services (CMS) is one of the largest healthcare payers in the United States.
13. Care coordination
Care coordination in the primary care practice involves deliberately organizing patient care activities and sharing information among all of the participants concerned with a patient's care to achieve safer and more effective care. This means that the patient's needs and preferences are known and communicated at the right time to the right people, and that this information is used to guide the delivery of safe, appropriate, and effective care.
14. RWD, Real-world data
Real-world data are the data relating to patient health status and/or the delivery of health care routinely collected from a variety of sources. RWD can come from a number of sources, for example
- Electronic health records (EHRs)
- Claims and billing activities
- Product and disease registries
- Patient-generated data including in home-use settings
- Data gathered from other sources that can inform on health status, such as mobile devices
15. RWE, Real-world evidence
Real-world evidence is the clinical evidence regarding the usage and potential benefits or risks of a medical product derived from analysis of RWD. RWE can be generated by different study designs or analyses, including but not limited to, randomized trials, including large simple trials, pragmatic trials, and observational studies (prospective and/or retrospective).
16. IDN, Integrated Delivery Network
An integrated delivery network (IDN) is a formal system of healthcare providers and facilities that offer both health care services and health insurance plans to patients in a defined geographic area (i.e. a defined patient population).
In an IDN, a set of physicians work with hospitals to form a healthcare ecosystem where people can receive any type of care they need from one single “brand” of healthcare provider.
17. Post-acute care
Post-acute care includes rehabilitation services that beneficiaries receive after a stay in an acute care hospital. Depending on the intensity of care the patient requires, treatment may include a stay in a facility, ongoing outpatient therapy, or care provided at home. Post-acute care settings include inpatient rehabilitation hospitals and units, long-term care hospitals, skilled nursing facilities, and home health agencies.
18. CIN, Clinically Integrated Network
CINs as individual providers and health systems that are collaborating strategically to do three things: 1) improve patient care, 2) decrease the cost of care and 3) demonstrate their value to the rapidly changing market.
A CIN can be a joint venture between a health system and providers, between provider partners only, or can operate as a subsidiary of a health system– which requires each provider member to sign a separate legal agreement to be part of the CIN.
19. Care management
Care management refers to a comprehensive suite of services and activities that help patients with chronic or complex conditions manage their health. Care management’s overarching goal is to improve patient health. To get there, the model also aims to improve care coordination, reduce hospital visits and boost patient engagement. Care management software can significantly support healthcare providers meet those goals.
20. Critical Access Hospitals
A critical access hospital (CAH) is what it sounds like: a hospital that provides needed access to patients who might otherwise have a difficult time reaching a hospital. In order to be certified as a CAH, a hospital must be located in a relatively rural area. Rural seems to be defined by the hospital’s lack of proximity to other hospitals or CAHs. Generally, a CAH must be 35 miles away, at minimum, from another hospital or CAH in order to qualify for the status. There are over 1,300 hospitals in the United States that have been certified as CAHs. You can see a map of their locations at the Rural Assistance Center website.
21. Community Oncology
A community oncology practice is a private physician owned business not part of a hospital or academic or medical teaching institution. The community oncology practice may be only a single oncologist, with one office and a support staff of physician extenders, nurses, pharmacists, or pharmacy technicians and other staff. The largest community oncology practice in the country is in Texas and has over 400 physicians on staff and over 25 satellite offices. There are community oncology practices in almost every state, in rural locations, and in the largest cities.
22. P4P, Pay for Performance model
Pay for Performance in healthcare (P4P), also known as value-based payment, comprises payment models that attach financial incentives/disincentives to provider performance. P4P is part of the overall national strategy to transition healthcare to value-based medicine. While it still utilizes the fee-for-service system, it nudges providers toward value-based care because it ties reimbursement to metric-driven outcomes, proven best practices, and patient satisfaction, thus aligning payment with value and quality.